RCPA Holds 2023 Legislators’ Breakfast
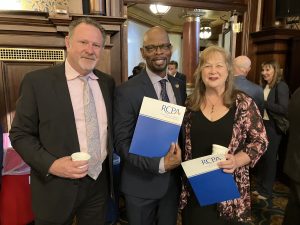
RCPA held a Legislators’ Breakfast at the Capitol today, April 26, to discuss issues related to health and human services as well as to meet the new legislators. We thank everyone who attended, including Rep. Mike Schlossberg and Rep. Joanne Stehr, who both spoke with RCPA President and CEO Richard Edley.


RCPA Policy Directors were also in attendance. Policy Director Jason Snyder spoke with Sen. Christine Tartaglione, while Policy Directors Jim Sharp and Carol Ferenz spoke with Rep. Stephen Kinsey. Carol Ferenz then spoke with Rob Labatch of RCPA member Hope Enterprises, Inc. and Rep. Paul Takac. Policy Director Melissa Dehoff was also busy speaking with several representatives and members, including Rep. Lisa Borowski, Rep. Tarik Khan, Bridget Lowery of RCPA member Success Rehabilitation, Inc., and Jack Poplar of RCPA member Acadia Inc.



Alongside RCPA Policy Directors was Board Member Susan Blue of Community Services Group. She spoke with several legislators, including Rep. Nancy Guenst, while Policy Director Jack Phillips spoke with Nick Troutman, who serves as Chief of Staff for Senator Yaw.


RCPA thanks its members who attended and spoke one-on-one with those who can shape the policies affecting health and human services. Employees of RCPA member Chimes Holcomb made an appearance, in addition to Hope Enterprises, Inc., Acadia Inc., and Success Rehabilitation, Inc.


We thank everyone who attended and supported our Legislators’ Breakfast. It was an incredible experience discussing health and human services in the Commonwealth while meeting all the new faces! We look forward to continuing to work with the legislature.
PA Health, Human Services Providers Jeopardized by Funding Needs, Workforce Shortages
RCPA Annual Membership Meeting and PAC Golf Fundraiser — May 10
Last Chance to Register for Integration of BH and PH Services in PA: A Legislative View — April 28
2023 RCPA Capitol Day Highlights the Need for Funding for Health and Human Services
RCPA hosted our 2023 Capitol Day today, April 24, on the steps of the Capitol outside the Main Rotunda. Our rally focused on the need for funding in health and human services to combat the workforce crisis as well as an increase in training for staff and advocacy for telehealth, amongst other issues. You can view our 2023 legislative and administrative priorities here.

 Those who spoke at our rally included RCPA President/CEO Richard Edley (left) and RCPA SUD Treatment Services Policy Director Jason Snyder (right). The two spoke of insufficient funding, overbearing regulations, and other issues deeply affecting human services providers in the Commonwealth.
Those who spoke at our rally included RCPA President/CEO Richard Edley (left) and RCPA SUD Treatment Services Policy Director Jason Snyder (right). The two spoke of insufficient funding, overbearing regulations, and other issues deeply affecting human services providers in the Commonwealth.
Also in attendance were Rep. Mike Schlossberg (left), Rep. Dan Miller (center), and Rep. Doyle Heffley (right). We thank them for their attendance and for showing support to those who work in health and human services.




 Lloyd Wertz, Executive Director of Family Training and Advocacy Center (left), and Sherri Landis, Executive Director of The Arc of PA (right), were also in attendance. Both spoke passionately on the challenges facing those working in health and human services.
Lloyd Wertz, Executive Director of Family Training and Advocacy Center (left), and Sherri Landis, Executive Director of The Arc of PA (right), were also in attendance. Both spoke passionately on the challenges facing those working in health and human services.
Last but not least, we thank those on the ground who do the hard work and who came out to support our efforts today. We especially thank Conference of Allegheny Providers (CAP) and KenCrest for their advocacy! We hope these efforts bring light to the work that you do for your communities.


Pennsylvania Previews Master Aging Plan

CHC-MCO Resource Document Now Available
Pa. Rep Holds Hearing on Workplace Age Discrimination
RCPA 2023 Capitol Day and Rally Information
RCPA will be hosting our 2023 Capitol Day on Monday, April 24. During the day, RCPA will hold a press conference and rally on the steps of the Capitol outside the Main Rotunda between 12:30 pm – 1:30 pm. Invited representatives for the press conference include Rep. Dan Miller, Rep. Mike Schlossberg, Rep. Donna Oberlander, Rep. Bridget Kosierowski, Rep. Doyle Heffley, and Rep Stephen Kinsey. Those invited will speak alongside Richard S. Edley, President and CEO of RCPA, and RCPA Policy Directors. If you have not registered for this event, please register here.
RCPA requests members schedule appointments with their Senate and House legislators to discuss the state budget, legislation, and regulations. Members may access the following documents to be used in their meetings with their representatives:
- RCPA Legislative and Administrative Priorities
- Early Intervention Position Paper
- ID/A Downsizing Infographics
- ID/A Workforce Compensation Survey
- ProVantaCare Community HealthChoices RFI Response
- RCPA Brain Injury Service Landscape Infographic
- RCPA Community HealthChoices RFI Response
- RCPA Mental Health Fact Sheet
- RCPA Value-Based Purchasing Survey Brief
Copies of materials will also be available at the Capitol Rally.
Members can visit the Pennsylvania Capitol website to find parking information and maps. If you have questions regarding our 2023 Capitol Day, please contact Jack Phillips.
We look forward to seeing you on April 24!
















