Nursing Shortages and Skilled Unit Closures Are Slowing Down Discharges at Pittsburgh Hospitals: Several RCPA Members Quoted
Pennsylvania Program Sends Out 10,000 Anti-Overdose Medications
ANCOR Stateside Report — August 29
OLTL Issues Act 150 Reevaluation & Level of Care Redetermination Procedure
The Office of Long-Term Living (OLTL) has released a communication that provides clarification to Act 150 Service Coordination entities on the Act 150 to Community HealthChoices (CHC) Waiver Transfer procedure. This procedure outlines the steps the Act 150 Service Coordinator (SC) should take once the participant has been confirmed nursing facility clinically eligible (NFCE), and a financial eligibility determination is needed to confirm if the participant is to transfer to the CHC Waiver.
As detailed in the Act 150 Guidelines, the reevaluation process is to be conducted at least once each year within 365 days of the first level of care determination and each subsequent year.
Additional questions should be sent to OLTL’s Division of Fee for Service Operations electronically.
Pa.’s Telemedicine Waivers Create Confusion
RCPA Member Partners for Quality Announces Jen Dayton as Executive Director of Citizen Care
Don’t Delay! Early Bird Registration for Together! Ends Sept. 9
Registration for the RCPA Conference 2022 Together! is now open! Together! will be held October 11 – 14, 2022, at the Hershey Lodge in person this year. Be sure to register soon, as early bird rate is available now until September 9, 2022.
We are excited for the lineup of speakers who will be presenting at this year’s conference, as there will be pertinent information available and discussed for all service areas. Workshop sessions include:
- Northwest Pennsylvania Veteran Suicide Prevention Program
- Presented by Greg Griffith of University of Pittsburgh PERU as well as Mandy Fauble and Stacey Buettner of UPMC Western Behavioral Health at Safe Harbor
- Evaluating the Use of a Digital Therapeutic to Improve Client Engagement and Access to Post-Discharge Outcomes
- Presented by Jennifer Irvin and Winnie Nagle of Pyramid Healthcare, Inc.
- Father Engagement Through the Eyes of the Child
- Presented by George Fleming and Misty Woody of Allegheny Family Network
- You Have All the Data — Now What? How to Leverage Data to Demonstrate Quality
- Presented by Rayni McMahon of Consulting for Human Services, LLC.
- Technology Solutions to Elevate the Level of Independence for Individuals With Disabilities
- Presented by Shaleea Shields of LumiCare
- Possibilities of Play — Board Games for Skill Building
- Presented by Jack Berkenstock Jr. of The Bodhana Group
- How Supportive Care Services Addressing Social Determinants of Health Impact Quality of Life
- Presented by Mia Haney and Phil Wilkins of Modivcare
Be sure to check out the entire list of sessions in our brochure, and note that sessions will be recorded to allow participants to take advantage of sessions after the event.
In addition to an amazing roster of speakers, our 2022 Conference will have an exciting array of sponsors and exhibitors. We thank those who have committed to our conference thus far! If you are interested in sponsoring or exhibiting, visit here for more details.
We’d like to give a special shoutout to our Connections Hall sponsor Beacon Health Options as well as our Welcome Reception sponsor UPMC Community Care Behavioral Health Organization. Thank you for your support!
Questions about the conference may be directed to Carol Ferenz or Sarah Eyster, Conference Coordinators.
Monkeypox: What You Need to Know — Webinar August 31
Learn the facts about the symptoms, prevention, and what to do if you or someone where you work gets sick. This webinar will include presentations by leaders and clinicians from the Department of Human Services (DHS) and the Department of Health (DOH), as well provide an opportunity for Q&A.
Please forward the webinar invitation along to any other relevant stakeholders in your network. For those unable to attend live, a recording of the session will be made available.
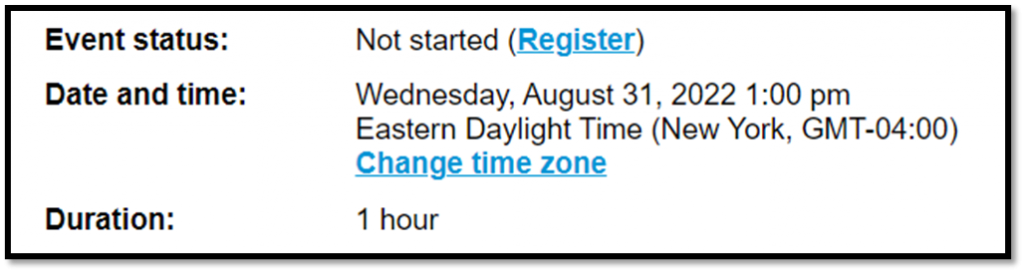
Visit HERE to register for this webinar scheduled for Wednesday, August 31 at 1:00 pm. When registering for the event, you must fill out the registration information by clicking “Register” on the left side of your screen as shown below.
Revision to the Enhanced Communication Rate for Services
ODP Announcement 22-099 provides a revision to the rate for the Office of Developmental Programs (ODP) services for enhanced communication. The enhanced communication rate is available for services from providers who have proficient signing staff to serve signing d/Deaf individuals or utilize PA registered, certified Sign Language Interpreters during service provision.
Attachment A is available to explain the differences between having staff who are fluent in American Sign Language (ASL) versus using an ASL Interpreter.
Providers who wish to request an enhanced communication rate must complete either the: Enhanced Communication Rate Request Form (Signing Staff) — Attachment B, or Enhanced Communication Rate Request Form (Sign Language Interpreting Services) — Attachment C.
Questions about the contents of this announcement may be directed to the ODP Deaf Services inbox. This communication obsoletes ODP Announcement 20-011, Revision to the Enhanced Communication Rate for Services.